Explain it like I'm 5: Prescriptions Part 1: Formulary
This is number... 5 I think? This one will actually be in 3 parts. This is Part 1 on pharmacies and goes over how to find out on the formulary if your drug is covered.
So, other than appeals, anything to do with pharmacy trips people up. This is in part because the insurance companies switch their formularies all the time. True story, had to do a prior authorization for a medication, it took over a month and a half to get the approval, and by the time it was approved, it went from $0 copay to a $700 copay the day after. It’s something that people aren’t aware of. You can ask the company to send you a formulary, or find one online through the company website with your other resources.
I will be doing a seperate newsletter on Step Therapy and PBMs, as I am being yelled at about this being too long for an email.
Anyway, let’s begin.
Formulary basics
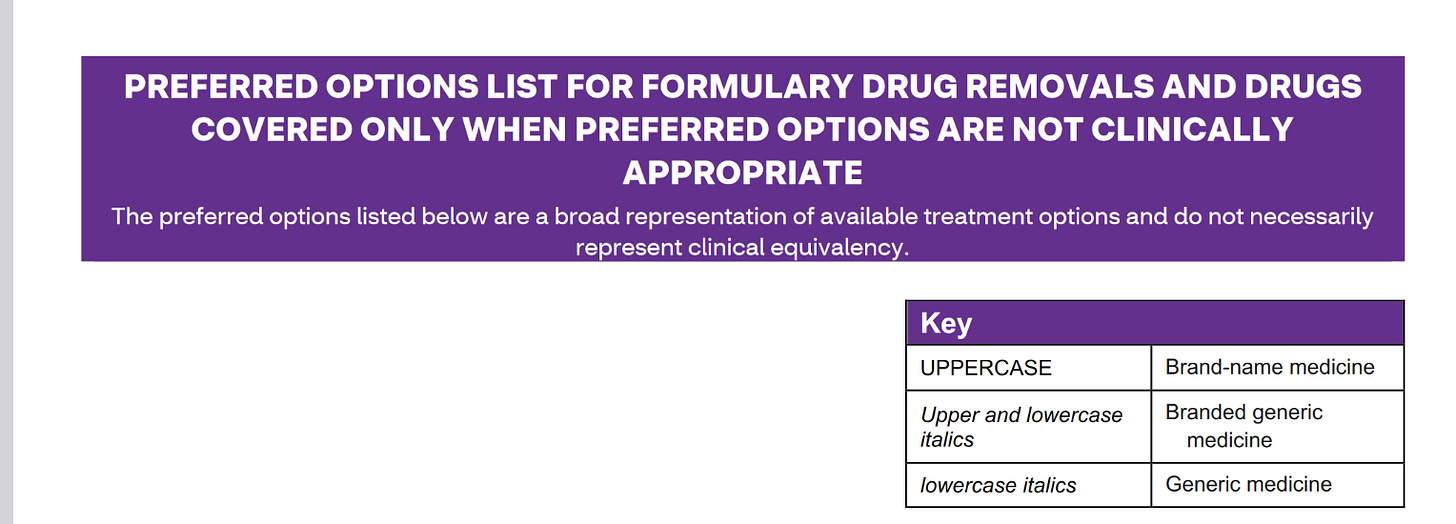
So, the formulary is over 200 pages. Here is the link. You can also get this in a paper copy mailed to your house, but it will be a pain in the ass finding the the drug. At least on a digital form you can ctrl + F to find things easier.
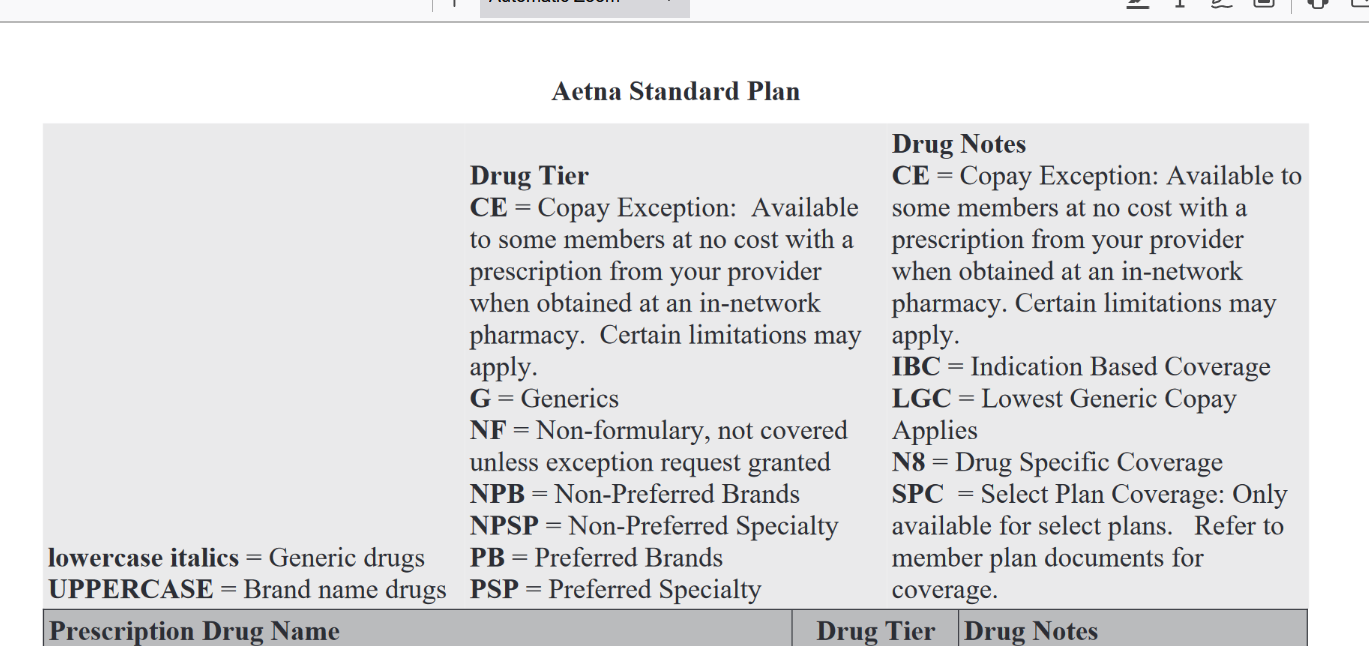
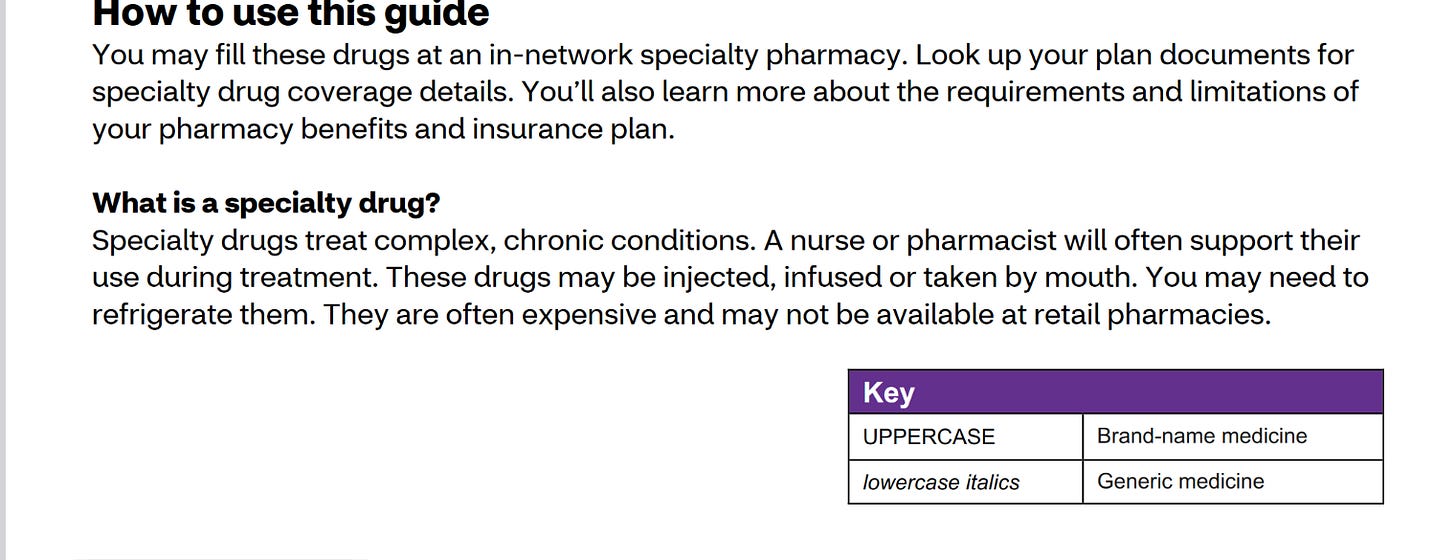
And of course, because this stupid place loves acronyms and bullshit, this is the legend for the formulary. Yes, it is dumb and confusing on purpose.
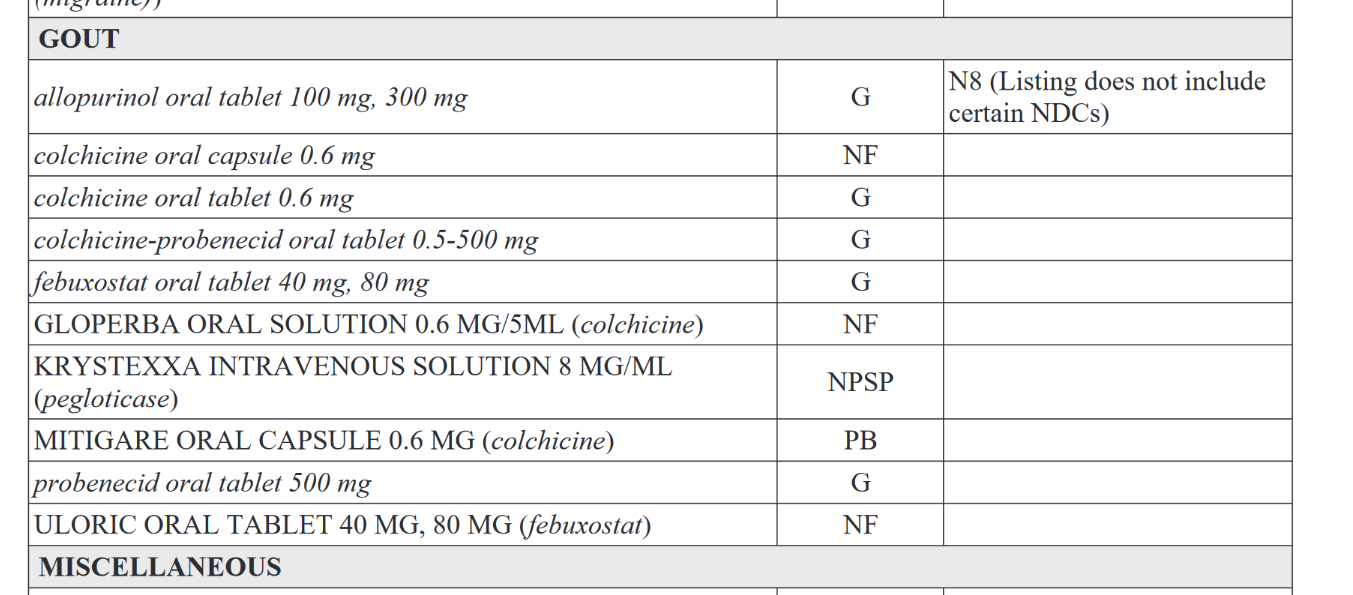
Here is an example.
So, if we look at this list and the legend at the top, if you’re taking KRYSTEXXA, which is a name brand drug as it is in all caps, you can see that the drug is covered, but it’s NPSP, which means non-preferred specialty drug. It’s covered at a lower rate than the MITIGARE, which is a preferred brand.
I’m not privy to how they decide what is and isn’t covered, but considering that CVS owns Aetna and CVS Caremark, I can assume it’s money-related.
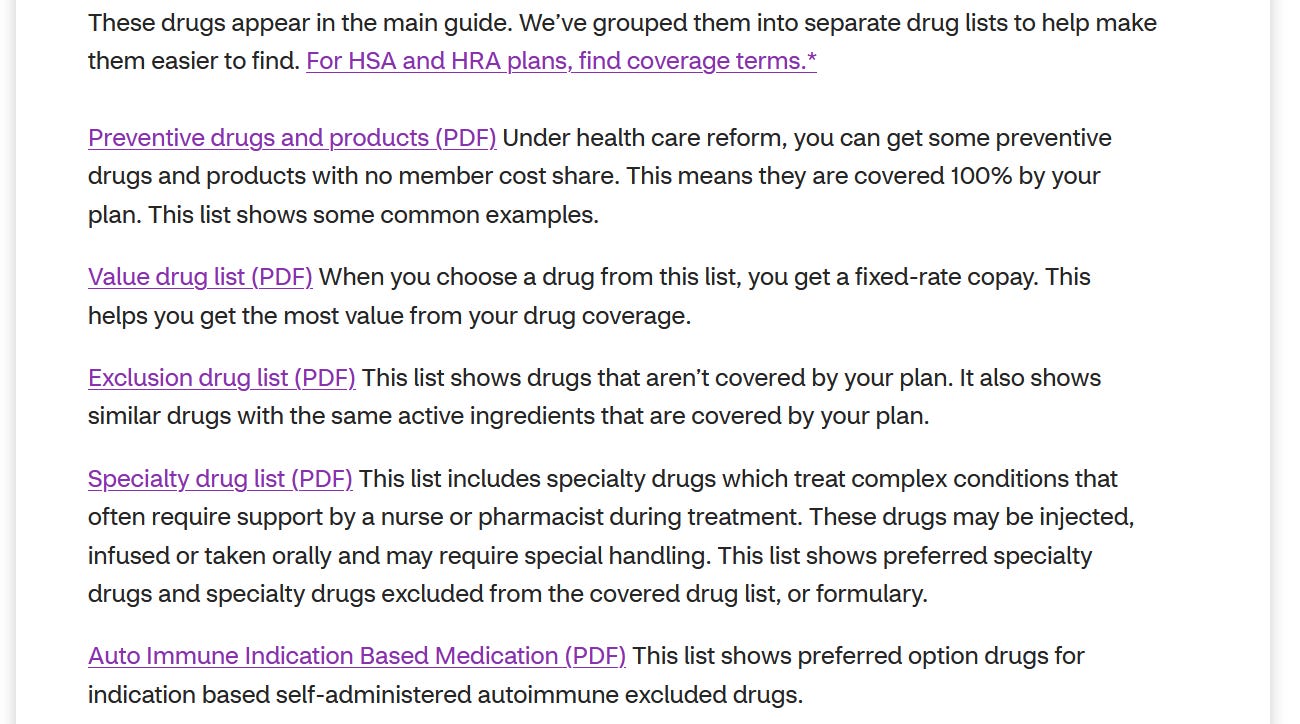
And this is the standard formulary. There are others, too! Lists upon lists upon lists.
So each of these are more information for you. I’m going to go over each list. They are the same drugs listed, but they are now grouped so you’re not searching all over.
LIST 1: Preventative
The drugs in this list are required to be covered with no copay and no cost.
It is only with prescription, so there are still going to cost money if they’re bought OTC.
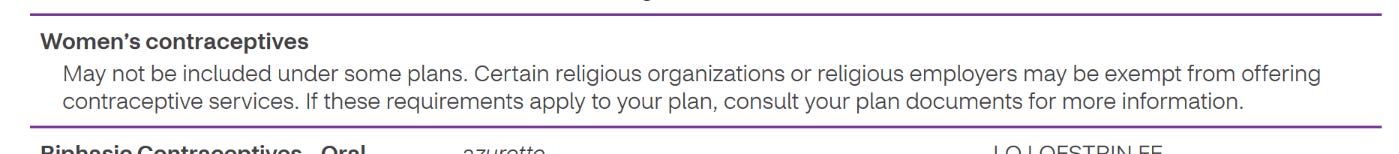
This is important if you have certin health conditions that require the medication on this list. It’s important to note that multiple forms of contraception are on the list. Of course, your company can file for religious exemption which means this:
Because of course, the employer has complete control over your insurance. (A lot of employer-sponsored plans are bespoke, so your insurer helps with creating a plan for employees.
LIST 2: Value Drugs
These are the drugs that are covered at a “preferred” rate.
So they will push to have these drugs covered over others, and they will cost less depending on factors like tier, copay, deductible, and other aspects of the plan.
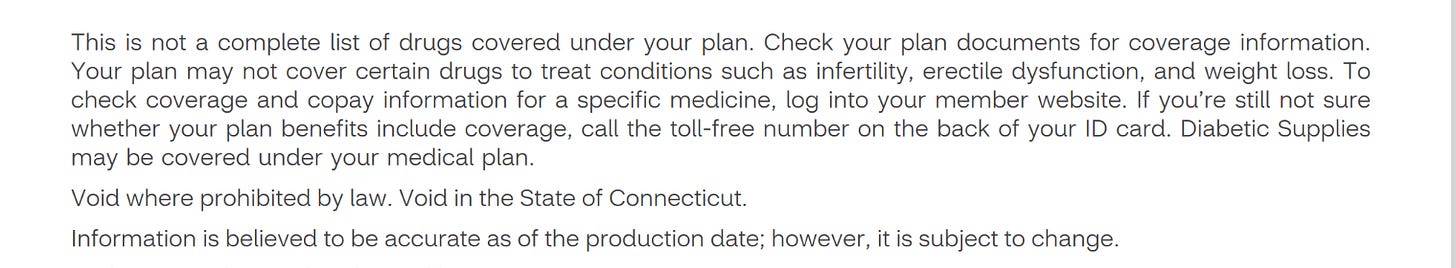
LIST 3: Exclusion list
This is proably the most important one. This list shows what drugs are not covered except under specific circumstances. This changes a lot. And if you are not aware, you could end up picking up a prescription that was $0 last month and now is $500 because it was added to this list. This is a big deal when it comes to name-brand drugs. And it’s a pain in the ass to get drugs covered. I will be addressing that in Part 2 of this series, as this goes hand-in-hand with Step Therapy.
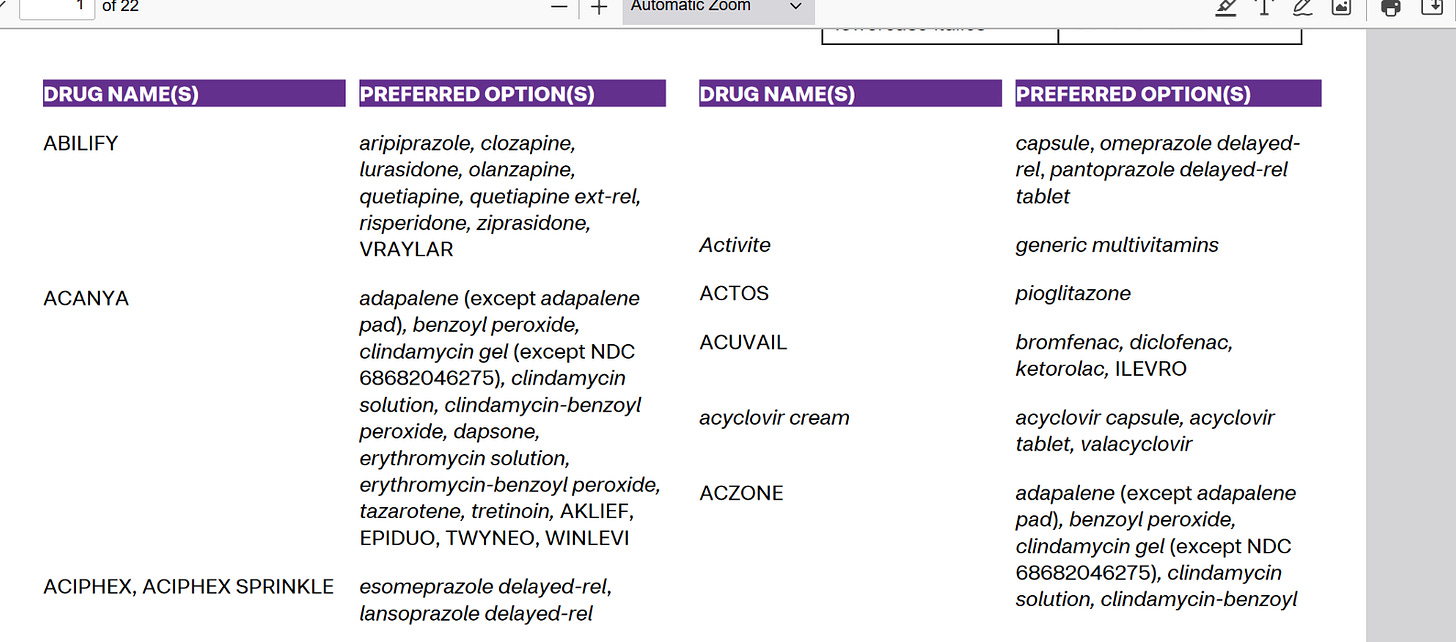
So it looks like this:
All caps drugs on the left are the name brands/generics that the insurance will not cover, and the right are the drugs they will cover. So if you were on Abilify, you will be switched to one of the generics (You know, the big sign at the pharmacy that says “We will switch out name brand unless otherwise stated”), and this is where step therapy comes in.
LIST 4: Specialty Drugs
This is for all the weird drugs. These are the ones typically without a generic version, and are for more complex conditions.
So these are going to be the more weird drugs. You will have to use a specialty pharmacy:
Specialty pharmacy refers to distribution channels designed to handle specialty drugs — pharmaceutical therapies that are high cost,[1][2][3] high complexity[3] or high touch.[2] High touch refers to higher degree of complexity in terms of distribution, administration, or patient management which drives up the cost of the drugs - Wikipedia Link
This makes sense in practice, but I will go over where this turns into an issue in Part 3 of this series, on Pharmacy Benefits Manager.
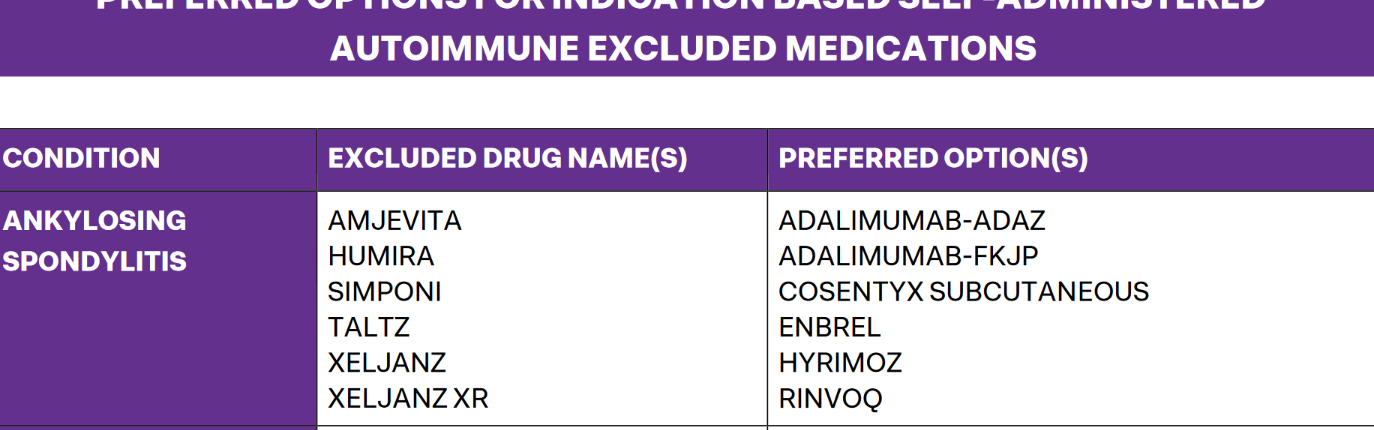
LIST 5: Auto-immune Indication Based Medication
This list is specifically to do with Auto-immune disorders. That’s because these drugs are incredibly expensive. So they get their own special list.
So, on the left is the excluded list, and right is preferred. Which means anything on the left is not covered by Aetna. And each insurer has a different formulary. You can find the information on these on each insurance website.
Anyway, this is part 1 of 3. Now that you know how to read it, we can get more into the nitty-gritty of it.
Thanks for reading!


Thank you for this!