Explain it like I’m 5: CPBs
CPBs (Or similar depending on the insurer) are part of how an insurer determines if a Prior Authorization is approved.
I was going to do this as a paid series, but honestly, I reflected on this and decided that this information really needs to be out there in a way that hopefully can be understood. If you found this helpful, please share. If you like this work, please consider becoming a paid subscriber.
CPBs, or Clinical Policy Bulletins, are part of what insurers use to approve or deny claims. Every insurance company has these, but they aren’t ever really spoken about. They are allegedly peer-reviewed to “Cut the amount of unnecessary care a patient may receive” As of right now, I can’t find any articles about how these CPBs affect rates of denial on authorizations and claims or if the CPBs are even accurate. Sources are sited at the bottom, but it would take forever for me to go through just one and look through the data.
So instead, I’m going to give you a brief overview of what they are, a few examples, and the URL for the 6 biggest insurers.
First off, What the hell is this?
As stated, CPBs, or the equivalent depending on the company, is basically a breakdown of how the insurance determines your eligibility for coverage for a certain procedure. It’s like a check-list, but it’s written in medical terminology and very difficult to understand for a lay-person. We were “discouraged” from discussing them because we are not doctors and for bringing them up to patients. Our SOP (standard operating procedures) changed all the time on these. One day we were allowed to directly send them to patients, other times were weren’t allowed to mention them, and sometimes we were allowed to fax them over, and sometimes we were not.
I think knowing how to access them and go over them with your doctor is important. Now, I don’t even have a degree, just some basic understanding of medical terminology from a prior employer, so please don’t ask me to decipher them. I’m just here to give you information for the next time you need a prior authorization or appeal, and if you’re particularly determined, checking out the source material and challenging them. Like I said, I am really limited here. These are freely available online from your insurer, and I will be providing links at the end.
CPB breakdown
Here is the first thing you see when you click on a CPB. I chose this one at random. The highlighted areas are where you can get information about the history of the CPB, information on when it was reviewed, when they will review it next, and definitions for the terms in the article. Circled is where you can find additional notes. Also, apologies for if this is slap-dash, because I am composing this, and all of my articles, on my phone.
Here is your table of contents. This is so you can jump around. I know you all know what this is, but if I’m going to be thorough, I’m showing you where it is. I have walked many a grandma through navigating our website, so better safe than sorry.
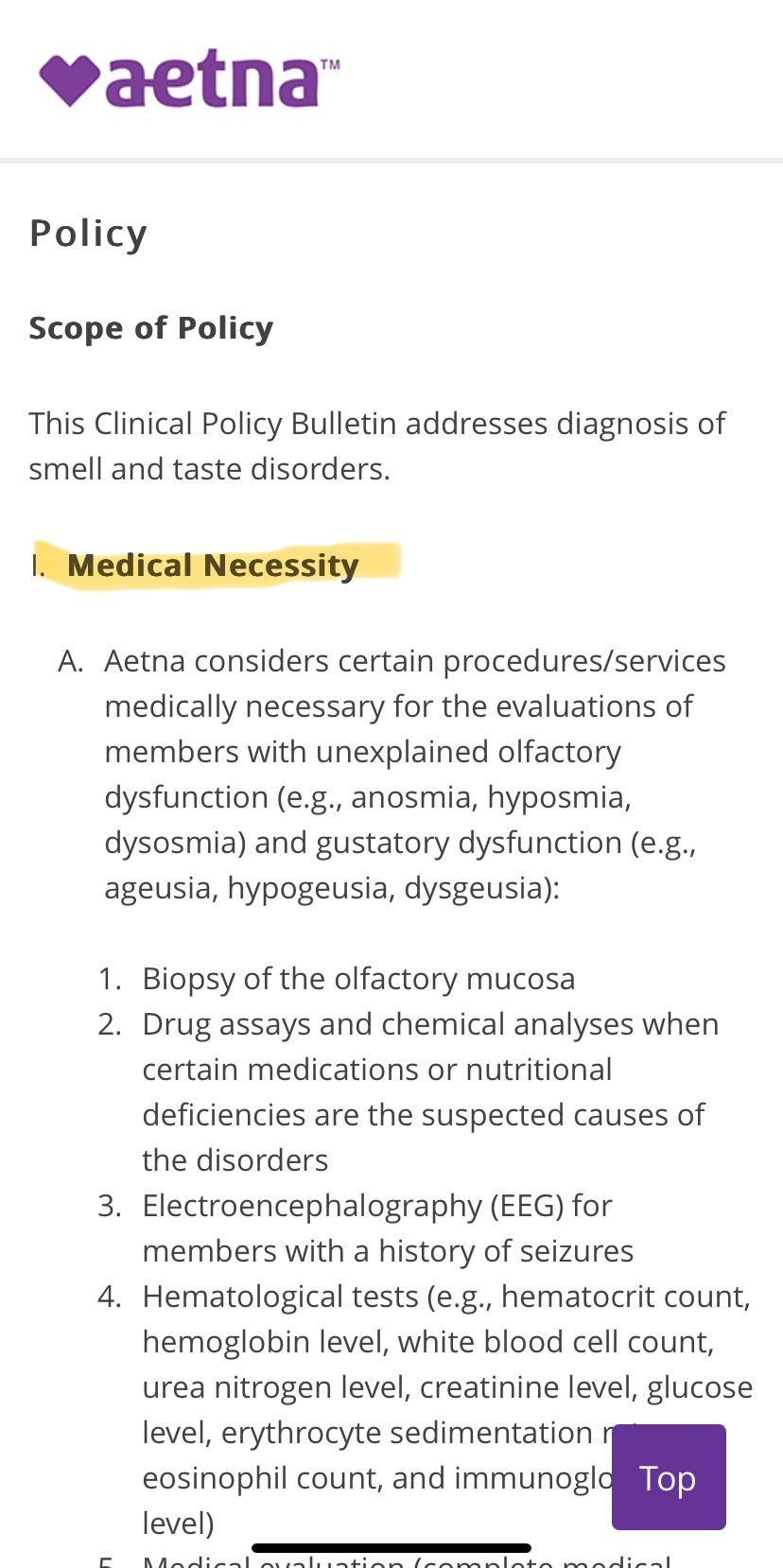
Here we get to the meat of it. This is where “medical necessity” is determined. Those famous words that everyone loves hearing on their denials. Here is the criteria that Aetna wants you to fit before they will cover the cost of care. These are the tests that they say they will cover. Now, obviously there is no guarantee, because in this day and age AI is being implemented in denials. But this information can be used in an appeal to hopefully make it easier for you to get coverage you are entitled to.
Again, please talk to your doctor, because this is a lot of terminology that you need a medical degree to really understand. I know looking at this makes the hamster wheel in my brain want to go into overdrive, and I am sure I am not the only one.
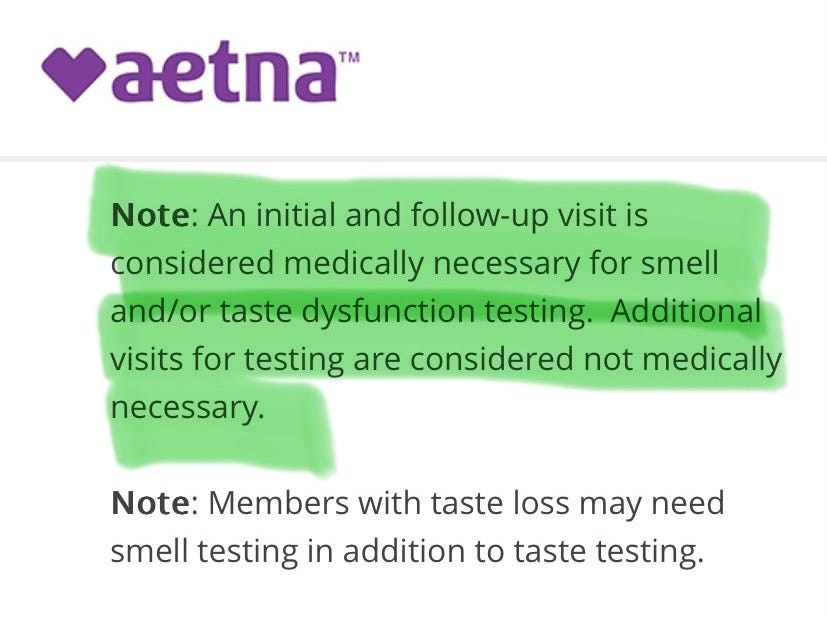
Now. I want you to take a look at this, because it is very very important. For this, you will only be covered for an initial testing, and a followup. There is the term “medical necessity” again. So, say you get a test, get an opinion, and the doctor wants you to receive additional testing. Maybe your case is complex. Maybe they can’t figure out what’s wrong. Well, you are shit out of luck.
This is when you would need to file a prior authorization, or you will not have a chance at the additional tests covered. I say chance, because we have all experienced this, myself included. This is how they get away with denying you, and it’s spelled out very plainly right here. All of these CPBs have this section.
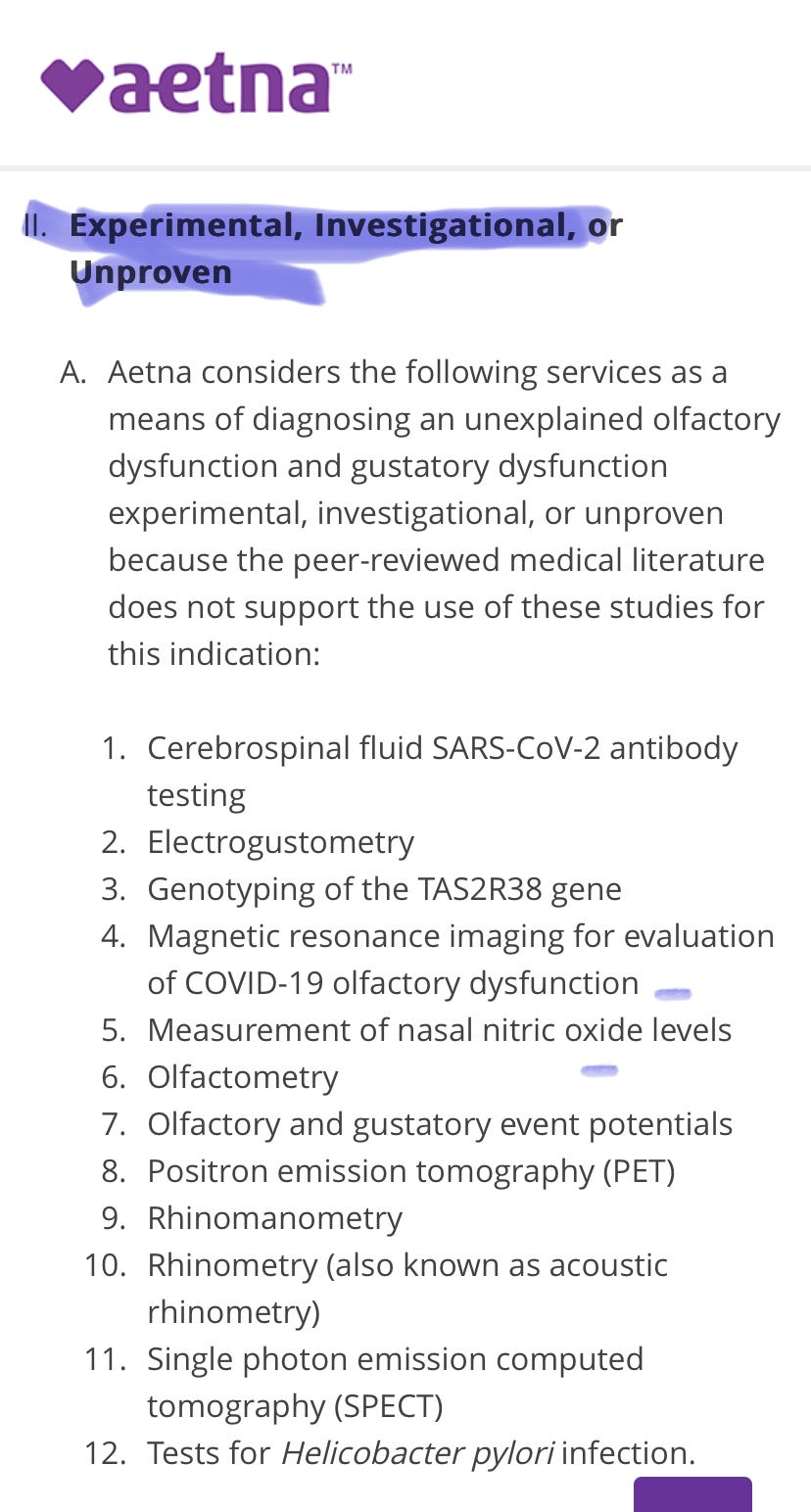
Here is where they tell you what they consider experimental. I wish I could tell you whether these are actually experimental or not. I honestly don’t know. But it’s good to look at this and research if you have the time, or ask your doctor their opinion. But this is the heading you want to make sure you review with your doctor if they plan on doing something “unconventional”
Here is a list of related policies. If you would like to go down a rabbit hole and read more of these, or just cross-check information.
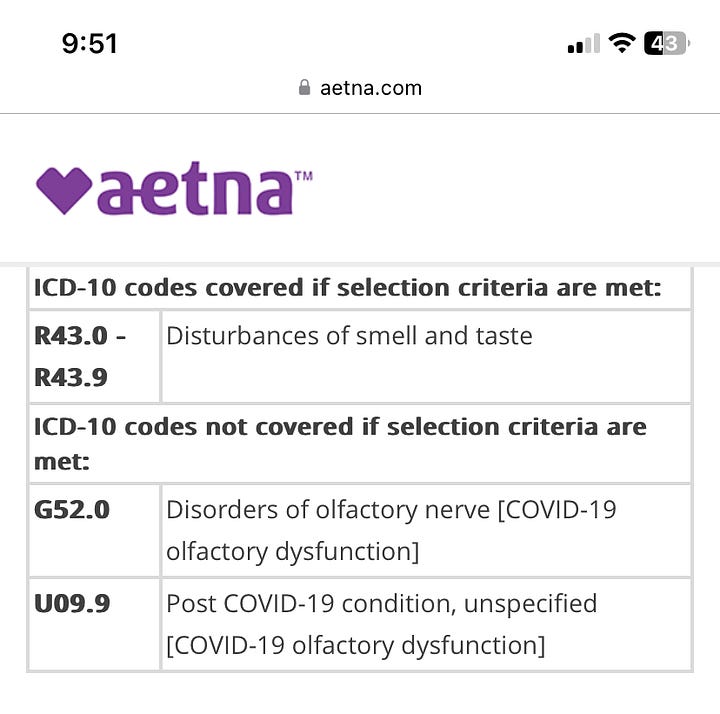
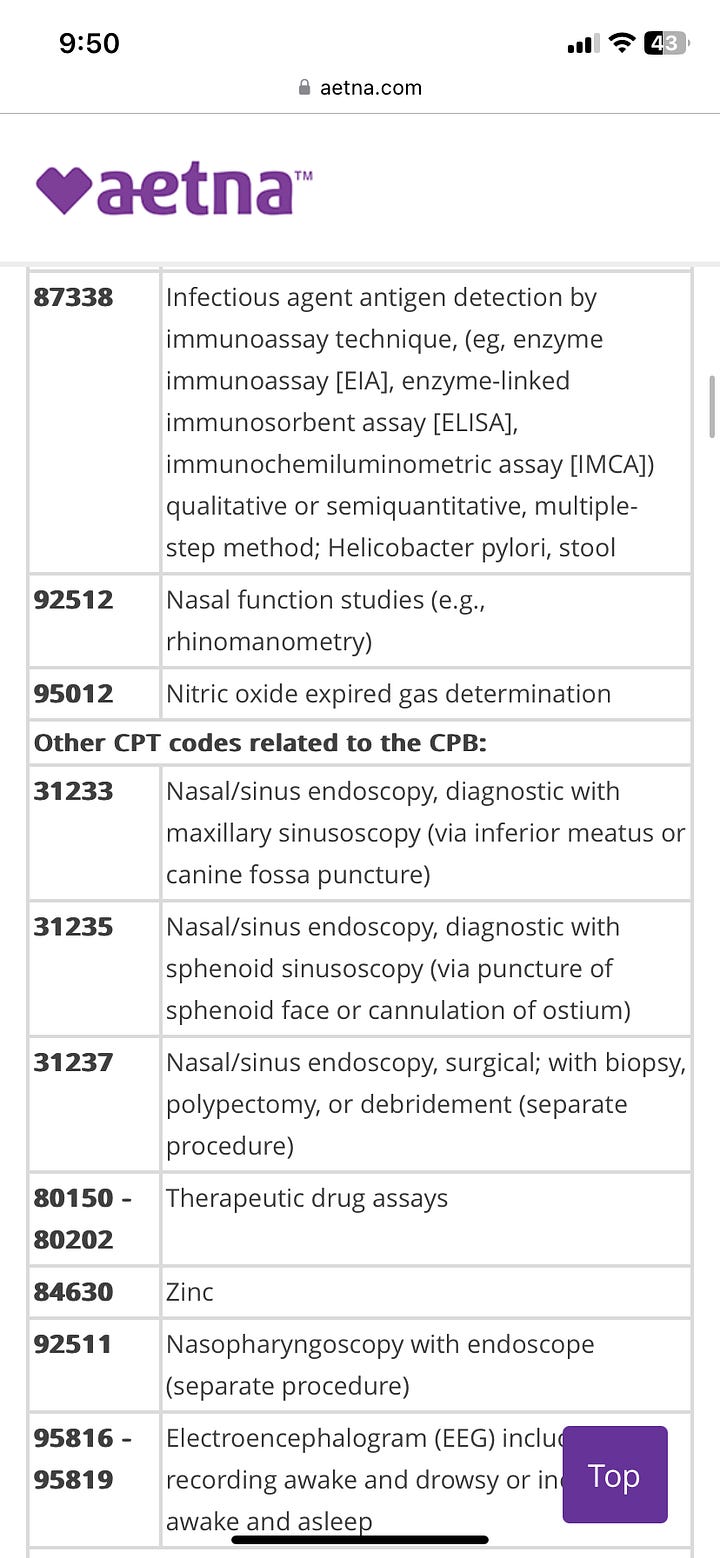
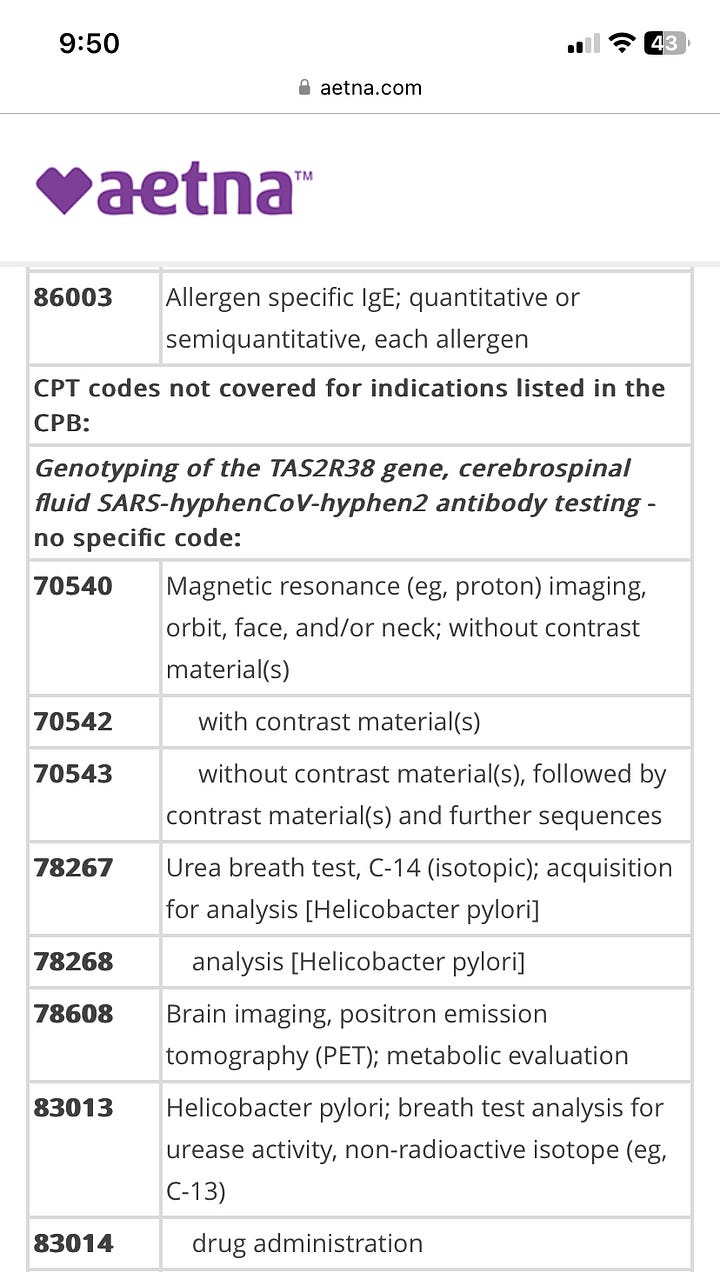
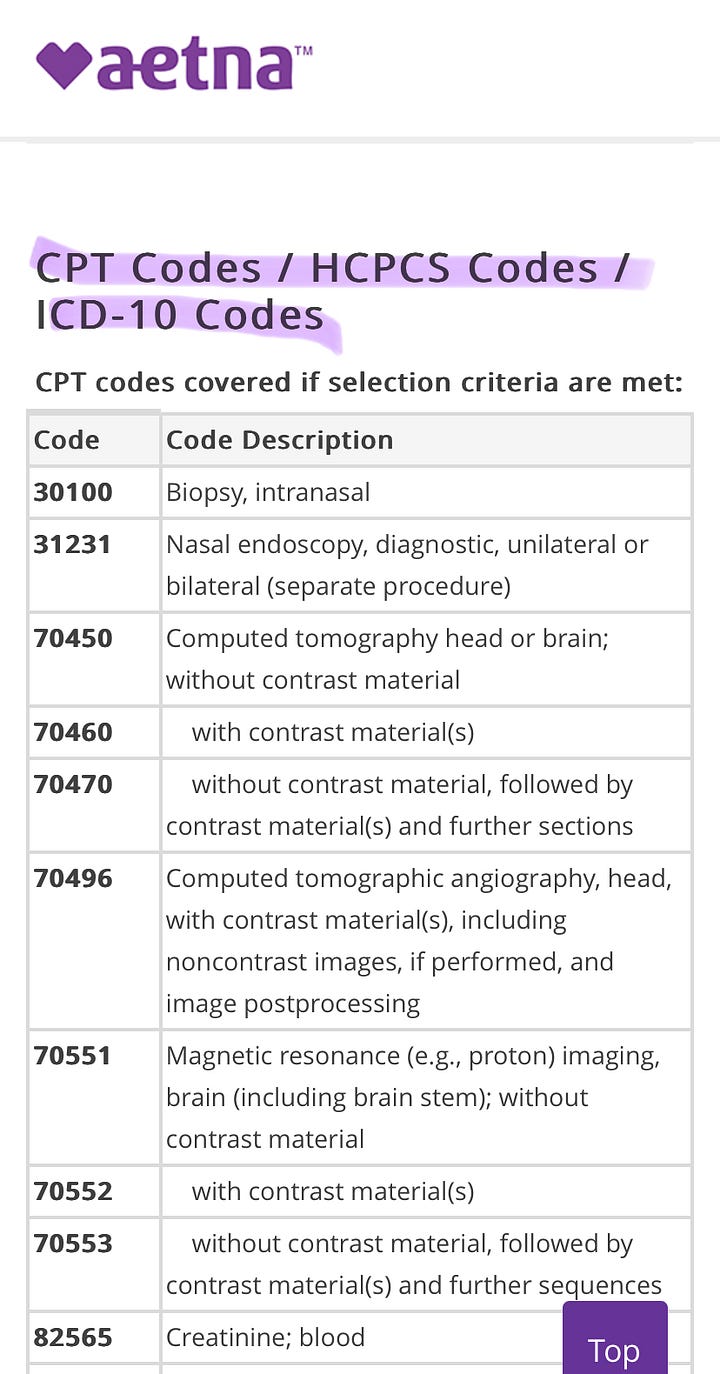
Here is a breakdown of what is considered for this procedure and what is not. This references billing codes for your medical bills. CPT codes and Diagnostic codes are something I will write about later on, but in short, this is what they use to categorize and bill for treatment. It shows you what CPT codes are and are not considered for this procedure or diagnosis. This is important because you can absolutely find this information on your medical bills and your Explanation of Benefits (the statement you get once a month that says “This is not a bill”. It will list all of the procedures you had, and includes the CPT and Diagnostic codes. I will be doing a breakdown of this as well in the near future) With this, you will be able to review the codes with your doctor for accuracy and to also add more fuel to an appeal. The thing that scares the insurance company is informed members. They don’t want you to know about this, and if you know what you’re looking at and what you’re doing, it makes it very easy to back them into a corner. I’m not saying it isn’t going to be a fair fight, but if you have information like this, it makes it a little less one-sided.
Now, you are armed with information.
The rest of the CPB goes into the background and then references. I’m not showing images of that here, because it’s a lot. And you can jump to it at your leisure using the table of contents. It’s a lot of extra information that is important, that I don’t feel is as critical as the first part.
This is the first part of what I hope to be a monthly breakdown of aspects of insurance for paid subscribers. This one I am making free because, frankly, this is not something that is talked about or mentioned. You hear a lot about prior authorizations, but you don’t hear how those determinations are made (not counting when AI is used) or what goes into this. And yes, this is mostly medical jargon that is hard to understand, because that’s the point. When I started working in Hell, I had no experience in this. Through training and also exposure, I now have a good understanding of how it works. And believe me, it only solidified my belief that we need a universal health care system. If you want more of this series, please consider becoming a paid subscriber. I know money is tight, so all of my other posts will be free, so if you just want some insight or to get the word out about the working conditions we deal with, please feel free to like and share.
And, as promised, here is a list of where you can find the clinical policy bulletins for the big 6 insurers:
Blue Cross Blue Shield (Anthem)