Explain it Like I'm 5: Appeals, Appeal Levels, and Tricks to Getting Your Healthcare Approved
So this one is going to be my favorite so far, because I get to help you get things approved by your insurance, whether they like it or not. Every dime you get covered brings joy to my black heart.
Appeals - Your best bet to get coverage
So! This part of my ELI5 series on insurance. This is going to be one of my favorites to date, because I will be assisting in forcing your insurer to cover your care. Some of these are through the company, but I’m also including other avenues, because while your chances of getting covered increase exponentially when you simply appeal according to the AMA, many people do not do this. And I understand. You’re trying to deal with a million other things, and trying to do one other stupid piece of paperwork is maddening, especially if you don’t understand what your looking at, or the terminology, or what to do.
Please read some of the other articles, talk to a friend, or fuck, send me a DM and I will walk you though it. I am not kidding, I live for this shit. I will gleefully assist you in your appeal. I fucking hate my job. And they absolutely hate you. And me. I do not get paid enough for my job, and being paid in blood money is gross. So, let’s get to it, shall we?
Appeal Basics: Different types of appeals.
There are different types of appeals. Most are familiar with prior authorization and attempting to get something covered in advance. When a prior authorization is denied, you are filing a “Pre-service appeal”. Simply put, you have not had the service, and you are trying to get a determination in advance. This will be the most common as this is what you have to do before you get a surgurey. I’m actually going through this right now, believe it or not. Thankfully, because I work in hell, it’s been very easy to speak to my doctors when I meet with them and go over my notes.
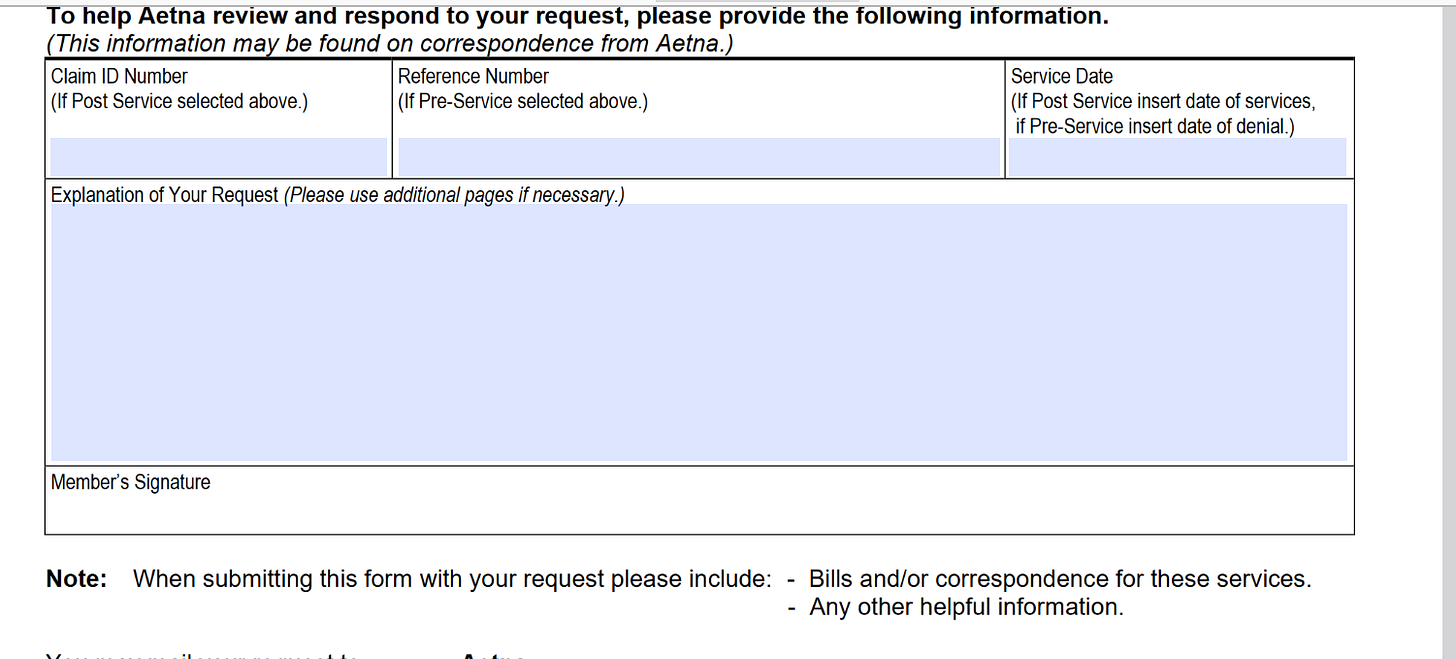
So this starts when you get a denial for a prior auth. Usually, these are bullshit. No lie, they are either done by an AI or someone wholly unqualified to make a decision. I’ve looked up credentials on denials. And now AI is being used. So it is a good idea to appeal. Now, it’s a pain in the ass to find the paperwork because… of course. I was able to locate the Aetna one. You can find it on the insurer’s app or googling “x insurance appeals form”
Here’s the form for Aetna:
So, first up:
YOU NEED TO PICK THE RIGHT INFORMATION ABOUT THE SERVICE YOU ARE TRYING TO APPEAL.
It seems so simple, but seriously, if you mess this up they will deny you right out and then you’re refiling the appeal and waitng another 30 or more days. If you think I’m kidding, I’ve seen it happen.
Since we are talking about a prior authorization, it would be a pre-service appeal.
Next you need to “explain your request”. While I would live to tell you to write “Cover my shit you fucking dicks, I pay too much for you to deny me”, you need to be specific. Go over your insurer’s utilization management (CPBs, I wrote about those as well). Be as detailed as possible. I mean it. Be gross if it helps. Make it look like you know your shit. That’s the best advice I can give. If you look like you know your insurance inside and out, you’re going to have an easier time getting approved. Why? Pretty sure it’s because they think you know enough to take legal action if they blow you off. Remember, these companies care about two things: Money and PR. There’s a reason that you probably didn't hear about all the lawsuits for CVS just last year (and one this year I haven’t gotten a chance to write about). So, make sure you are detailed and accurate. If you didn’t click on that link about the AMA, %80 percent of appeals are approved. So, you have a good shot of getting the care you need JUST by appealing. Again, look through my newsletters for anything that is Explain it Like I’m 5 and that will help. Or seriously, DM me, or ask me in my upcoming live (TBD date/time). Fuck these people.
Also, see if you can get a meeting to go over the paperwork and the CPB with your doctor before filing the appeal, because they will likely need more paperwork. I did that whenever I needed an appeal or prior auth. It is very helpful. Especially since you need to make sure your medical records match. This will be a big step in getting you the service you need.
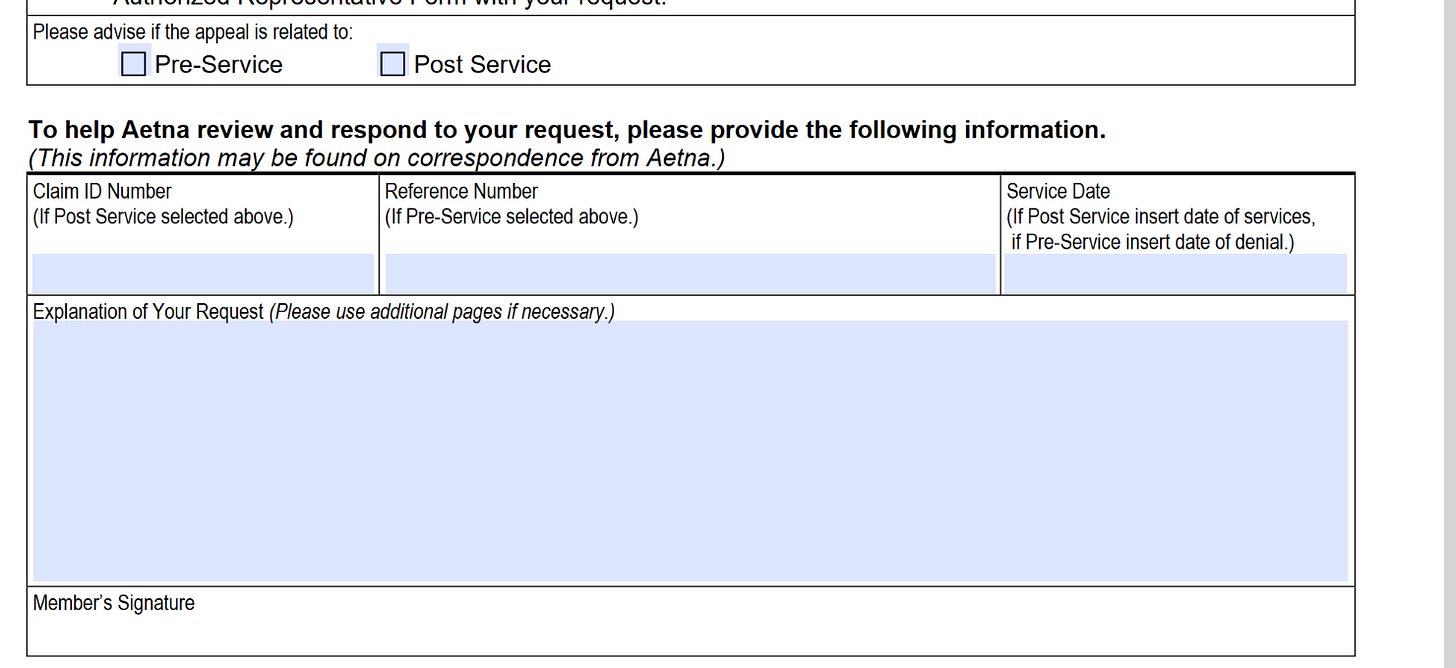
Post-Service: When a claim is denied.
Posting this page again, but now we’re looking at the second box:
So, post-service is when a claim is denied. So, to simplify: You get a procedure, you think you got everything taken care of. Then you get your EOB and you see that your service was denied. You now owe a ton out of pocket. The EOB says the proceedure was denied. This is when you would check “post service” on your appeal. You can also ask the attending physician for help with this. This is where your EOB is going to come in handy, because you will need those CPB codes. The rest of this is the same. You will still most likely need more documentation in the form of medical records. This may be a little harder, because they have their own “utilization management” guidelines, but you can get those online. Or What I learned from going through this my self is that 9 times out of 10, you meet all of the criteria, but it’s not “documented properly” and there’s not “enough proof of medical necessity”. I’m not kidding. That’s was part of the justification for my denial. They needs more evidence than a fucking homicide case, because you cost them money.
So that’s the basics. Now onto the more advanced.
I was denied on appeal. Now what?
So there are steps you can take. Going through the insurer is only the first step. There are a ton of additional steps. Again, this unfortunately is the way things are, because fucking of course we live in hell, and if you’re also trying to get your cancer treated, or attempting to treat your child’s horrific, debilitating illness, it can be really difficult to have the energy to deal with this bureaucratic bullshit.
Read this and his first article about his daughter. It’s fucking heartbreaking. I am not kidding when I say I fucking hate this job and the harm it causes.
So. The next step is a peer-to-peer. Or, a peer-to-”peer”, because it is often not the case that you're doctor will be speaking to a peer.
So, what Aetna says about it:
Peer-to-peer review: Aetna offers providers an opportunity to present additional information and discuss their cases with a peer-to-peer reviewer, as part of the utilization review coverage determination process. The timing of the review is prior to an appeal and incorporates state, federal, CMS and NCQA requirements.
And now what an actual doctor says:
“Peer to Peer.” That’s the euphemism insurance companies use for the frustrating ritual where a clinical physician, the one actually treating the patient, must plead their case to a doctor hired by the insurance company.
The goal? To get approval for something the treating physician has determined is necessary for their patient’s care—something the insurance company has deemed “not medically necessary.”
So, I’m going to agree with the doctor. And honestly, same with appeals. Let me show you:
Not to disparage anyone who only has a high school diploma (like me), but… shouldn’t someone working appeals have a medical background? You would think. But it’s real easy to copy and paste a spreadsheet and push the “deny” button. Also, another position that pulled up under this tag? Customer Service rep, because yes, I had to learn all of this shit too, and whatever the fuck else they wanted to tag on without extra pay. It’s why I’m able to write about it.
And don’t let the “coordinator” in the title fool you. I have a similar title, and it means less than any promise oozing out of a politician’s mouth. That position WILL be $17 bucks an hour. Again, ask me how I know?
Yeah, they lie out their teeth about wages. That range is to get around the pay transparency laws, because they hate their employees more than they hate their members. They made more money than god off of denying people care. They also bitched about it when it cost them too much money last year. It’s fucking embarrassing.
Anyway:
Back to peer-to-peer. Chances are, it’s a farce. The doctor on the other end is paid by the insurance company to deny over a missing comma. That is the next step, and you can and should absolutely take that as the next option, even if you know this. It just gives you fuel for your impending lawsuit.
You can also get an external appeal. For obvious reasons, we weren’t taught about this and they were never talked about. Here is a really helpful PDF for internal and external appeals. You can also just straight up file with a court. I had a really helpful document that I no longer have access to that details the final steps past peer review (it is absolutely involving the court though), but I have no access to those. (RIP old work computer) so if I can reach out to someone with that access I will be doing a part two with that information.
So, what are some other things you can do? Well…
Scare the shit out of them. I’m serious.
You know what they hate? Calling them on bullshit.
Real example. Friend of mine needed a bone cancer doctor. Not because he had bone cancer, but because he just got his chest cracked open at like 44 for heart surgery. He sent in a prior auth. The auth was denied, of course. He called up the the insurance agency. Immediately asked for the credentials of the person who issued the denial. If I recall, she was a pediatrician. He advised them that he was going to file a lawsuit. Guess who was approved the next day?
Qasim Rashad talks about this in his article. The second time the company tried to deny, he took to social media to shame them. He got a response almost immediately and his daughter’s treatment was approved.
So, first, when faced with a denial, ask if you can get the credentials of the person who denied you. They might push back, but press. Ask for the HIPAA compliance information. They are NOT allowed to hide this information, despite what they want you to think.
Look, be polite to the person. Don’t yell or be a dick. Everyone I worked with, for the most part, actually gives a shit and it makes us sick that we can’t do anything. Our job is to bear the brunt of the company’s decisions so they don’t have to be screamed at every day. Just be polite. 9 times out of 10 the representative has had the same shit happen. Anyway, if the representative can’t provide that info, you can escalate to a supervisor. You can also look online for the Hipaa compliance office.
Get the credentials and document it with the appeal. That’s one thing. It will absolutely scare the shit out of them. That’s one way.
Second, (especially if you have the doctor’s credentials), advise that you’ll be filing a complaint with the state. This link includes all 50 states. You can also reach out to your local reps office to send them the paperwork.
Do not take no for an answer. Shame them. Call your employer, call your state rep, your local news. This person gets it. If you are ill, you can have someone you trust fill out a ROI and Authorized representative form and they can help you. I am on file for my mom and spouse, because I know how to deal with this bullshit. And seriously, call your state rep’s offices. The staff there will absolutely help you. They have access to resources you do not. They’ll be able to cut through red tape for you. I have had to do this before, and they were able to get the problem solved.
Be a goddamn thorn in their side. Advise them that you will be complaining to every agency. I actually did this for a non-related issue and the issue was solved within 2 days. I know we have this idea that you’re a Karen if you do this, but you won’t be. Just don’t be a dick to staff.
And lastly, take to social media!! Post it everywhere! Reach out to the MANY publications that want to tell your story here and elsewhere.
I’m sure there is more,if you get creative. Public pressue works with these places, because they try to hide in PR. No, they really don’t want health care reform. They deny over 1 in 5 claims. If they could get away with more, they would.
But right now, none of these places can afford the PR disaster. Not after the roof was blown off in December. While UHC got the brunt, all of these places are on edge. You can feel it in every town hall. They know that if people start speaking out, it will make a splash. So, either you or a loved one, reach out. A lot of us are hear to listen and spread your story.
Anyway, that’s appeals! April I will be doing a piece on Formularies and PBMs. That will be “fun”
Stay safe everyone.
Aetna Employee #666







I've several friends and acquaintances that will love to know this, having been stuck with this problem. I'm already sharing this widely! Thanks!!
Thankful to be Canadian… 💋🇨🇦❤️